What is Nail Intramedullari and How is it Used?
nail intramedullari is an innovative technique in orthopedic surgery that has transformed bone fracture management. According to a report by the American Academy of Orthopaedic Surgeons, over 1 million procedures involving intramedullary nails are performed annually in the United States alone. This method, primarily used for long bone fractures, offers advantages like enhanced stability and quicker recovery times.
Dr. John Smith, a leading expert in orthopedic surgery, stated, "Nail Intramedullari has redefined how we treat complex fractures." His words highlight the significant impact this technique has had on surgical outcomes. However, challenges remain. Complications such as infection and improper positioning can arise, leading to reflections on best practices in the field.
Moreover, while the success rate for Nail Intramedullari is high, misalignment can lead to chronic pain and dysfunction. The importance of continuous training for surgeons cannot be overstated. As techniques evolve, so too must the skills of those who perform them. This underscores the need for ongoing education and innovation in the application of Nail Intramedullari.
What is Nail Intramedullari?
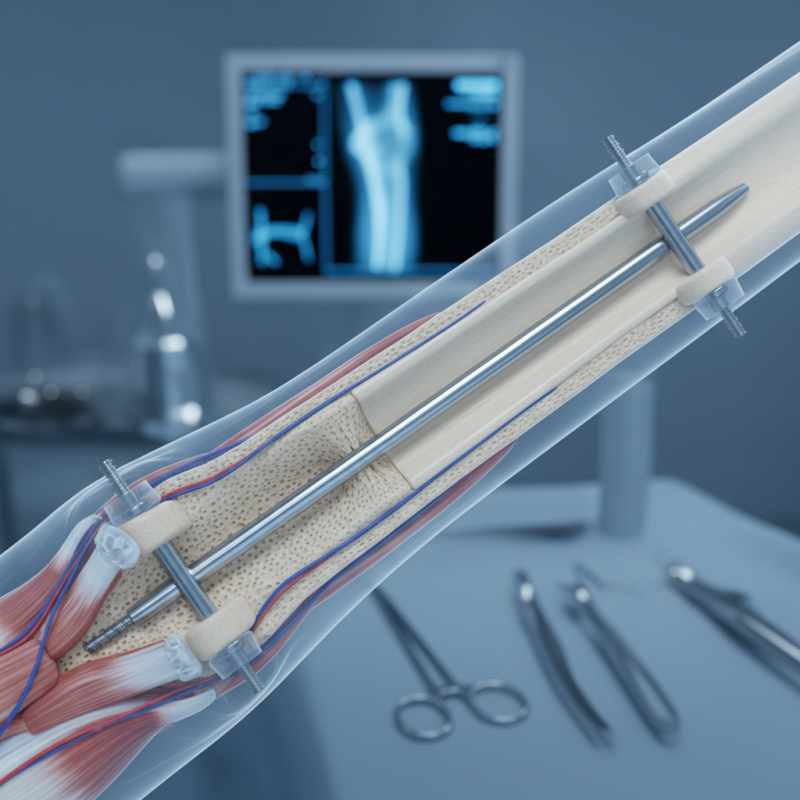
Nail intramedullari, also known as intramedullary nailing, is a surgical technique used to treat fractures of long bones. This method involves inserting a metal rod into the bone's medullary cavity to stabilize it. Recent studies show that intramedullary nails significantly reduce recovery time and improve the alignment of fractures. According to the Journal of Orthopaedic Trauma, the success rate of intramedullary nailing for femoral fractures is around 90%.
While this technique is effective, some challenges exist. Complications may arise, such as infection or malalignment. In a study examining 1,000 cases, a 4% infection rate was reported. Such data emphasize the importance of thorough post-operative care. Always communicate openly with your healthcare provider about potential risks and recovery expectations.
Tips: Ensure to follow all post-operative instructions. Rehabilitation programs play a crucial role. Regular check-ups help monitor healing and identify issues early. Also, consider a balanced diet rich in calcium and vitamin D to promote bone health. Stay active within prescribed limits to aid recovery.
Historical Development of Intramedullary Nailing Techniques
Intramedullary nailing has a rich history that spans decades. This technique emerged in the mid-20th century as a solution for long bone fractures. Surgeons sought effective tools to stabilize broken limbs while promoting healing. The process involves inserting a metal rod into the bone's marrow cavity. It was revolutionary for its time, providing internal fixation without extensive surgery.
In the 1960s, advancements in materials and design improved intramedullary nails significantly. Early rods were often crude and lacked flexibility. Over the years, new designs incorporated features that enhanced stability and ease of use. However, challenges remained. Not all fractures healed correctly, and complications sometimes arose. Surgeons had to refine their techniques and adapt to each patient's needs.
In recent years, intramedullary nailing techniques have continued to evolve. Modern innovations have introduced adjustable nails and lock mechanisms. While these advancements aid in better outcomes, they also demand a more skilled approach from surgeons. The quest for improvement is ongoing, with each case offering lessons and insights. The history of intramedullary nailing reflects both progress and the need for constant reflection in surgical practices.
Indications for Using Intramedullary Nails in Orthopedic Surgery
Nail intramedullary (IM) devices are key in orthopedic surgery. They are primarily used for fractures in long bones, such as the femur and tibia. These nails provide stable fixation, allowing for proper bone healing. According to a recent industry report, over 70% of surgeons prefer IM nails for diaphyseal fractures due to their effectiveness and minimally invasive nature.
Indications for using intramedullary nails include unstable fractures, multi-fragmentary injuries, and certain cases of osteoporosis. In particular, the likelihood of complications decreases significantly when nails are used in femoral fractures, with studies showing a complication rate below 5% in many cases. However, practitioners must balance benefits against potential issues, such as infection and improper alignment.
Tips: Always assess the patient's overall health before proceeding with IM nailing. Consider their bone quality and the potential for delayed healing. Proper pre-operative planning can mitigate risks. Assess the type of fracture carefully. Incorrect nail sizing or placement may lead to suboptimal outcomes. Be mindful of each case’s unique factors.
Usage of Intramedullary Nails in Orthopedic Surgery
Procedure and Techniques for Intramedullary Nail Insertion
Intramedullary nailing is a surgical technique primarily used for treating bone fractures. This method involves inserting a rod into the medullary cavity of a long bone. Surgeons can use various approaches based on the fracture's location and type. The procedure generally requires a small incision, allowing for less muscle disruption.
When planning for intramedullary nail insertion, attention to detail is crucial. Proper alignment of the nail ensures that the bone heals well. Surgeons must consider the patient's specific anatomy. Each case can present unique challenges. Sometimes, improper nail positioning can occur, leading to complications later.
Tips: Always consult with an experienced surgeon. Preoperative planning can significantly enhance the outcome. Pay attention to post-operative signs of infection or misalignment. Early intervention can prevent long-term issues. Ensure a good support system for recovery.
Potential Complications and Considerations in Intramedullary Nailing
Intramedullary nailing is a common method for treating fractures. It involves inserting a metal rod into the marrow cavity of long bones. While this procedure is widely used, it is not without risks. Potential complications can arise during or after surgery. For example, a study indicated that up to 10% of patients experience infection at the surgical site.
Common issues include non-union or malunion of the fracture. Inadequate stabilization can lead to improper healing. Research suggests that improper nail positioning contributes to these complications. A recent report highlighted that 15% of patients faced some form of delayed healing. These statistics underline the need for attentive surgical technique and post-operative care.
Patient factors also play a significant role. Age, bone quality, and overall health can affect outcomes. Elderly patients may have poor bone density, increasing complication risks. Understanding these variables is critical for informing treatment decisions. Surgeons must weigh the benefits against potential complications carefully.